Dr. Álvaro Monterrosa Castro, MD
Pelvic inflammatory disease
Pelvic inflammatory disease (PID) usually causes sequelae: Infertility, increased rate of ectopic pregnancy and chronic pelvic pain.
An RCGP study showed that the relative risk of PID among oral contraceptive users is half that of non-users. Since 1980, Senanayake and Kramen (103), analyzing seven studies, had asserted the same conclusion.
This protective effect is likely due to the thickening of the cervical mucus produced by the hormones present in the tablet, preventing the rise and spread of bacteria in the internal genital tract. As well as the decrease in menstrual flow. However, the exact mechanism of the protective effect is unknown.
Studies indicate that protection is limited to current users of oral contraceptives and women who have used them for at least twelve months, with protection disappearing shortly after stopping the method. Based on figures from the Women’s Health Study, it is estimated that combined oral contraceptives prevent 50,000 initial cases of PID and 12,500 hospitalizations per year due to its complications.
In women with PID studied by laparoscopy, it is shown that combined oral contraceptives, in addition to reducing the frequency, reduce the severity of pelvic inflammatory involvement.
(Read Also: Decrease in the Incidence of Ectopic Pregnancy)
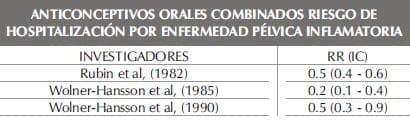
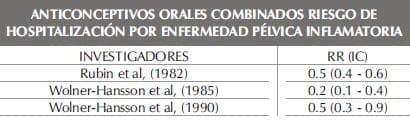
Risk of hospitalization for pelvic inflammatory disease
The use of combined oral contraceptives for at least twelve continuous months reduces the risk of hospitalization for pelvic inflammatory disease by 60%. This estimate of risk reduction is very similar for high-dose preparations and very low-dose pills (43).
The proportion of protection against inflammatory disease caused by gonococcus and that caused by other germs is not specified. In 1985, Washington and Collaborators (104) cite studies that suggest that oral contraceptive users have a double or triple risk of Chlamydea Trachomatis infection in the lower third of the genital tract. This event would be related to the possibility that oral contraceptive users were more sexually active than non-users, or to a deviation produced by the greater detection in women with cervical ectropion, which is related to the use of oral contraceptives.
The apparent increased risk of infection of the lower genital tract caused by Chlamydea Trachomatis in users of combined oral contraceptives requires further study, especially since the increased risk of cervicitis does not appear to be related to the risk of infection of the upper genital tract (105). . The estrogen-progestin association present in the pill is associated with a high prevalence rate of Chlamydea Trachomatis in the genital tract of young women.
The following table presents the relative risk of hospitalization for pelvic inflammatory disease in combined oral contraceptive users versus never pill users.